What patients want to know about COVID-19 when care providers aren’t available

An In-Depth Analysis of 2,000 Patient Interactions Across U.S. Healthcare Systems
COVID-19 is a previously unknown illness caused by a previously unknown virus (hence the “novel” coronavirus), so it shouldn’t surprise us that people are confused about core questions such as how the virus is transmitted, how it affects the body and what means of treatment exist.
What might be more surprising is that COVID-19 has revealed seams in our health system that we hadn’t previously noticed. The patient-doctor relationship is more significant than we may have realized. It appears that when we try to avoid face-to-face meetings, critical information becomes lost in transmission and important medical care goes undelivered.
Conversational AI company Hyro is in a unique position to reveal what people’s most burning questions about the virus are. Unlike other digital interfaces designed to help flatten the curve, Hyro’s conversational AI platform empowers healthcare enterprises to provide round-the-clock service to their patients using chatbots, voice assistants and virtual agents. In the face of the pandemic, Hyro built a COVID-19 solution, an AI-powered voice and text conversational agent which equips patients with actionable information and triggers a risk-assessment tool capable of evaluating a patient’s symptoms and likelihood of infection.
Hyro’s analysis of 2,000 patient conversations with their COVID-19 Virtual Assistants across American healthcare systems presents insights into the deep dependence that individuals feel towards their primary care providers, and the chaos and confusion that occurs when those providers aren’t available.
COVID-19 disrupted the patient-doctor relationship
Due to fears of infection, 42% of patients feel nervous about visiting a hospital and 45% feel the same about urgent care centers, with 72% of all patients agreeing that they have changed the way that they access medical services. Primary care centers are facing serious financial crises as a result of the sudden drop in patient admittance.
In theory, telehealth services should step into the breach and deliver information and support remotely. However, the results have been mixed. The volume of calls and messages sent to telehealth providers skyrocketed, especially among Medicare members who were previously mostly barred from such services. Emergency legislation lifting restrictions on Medicare reimbursements for telehealth led to an uptick in adoption of over 11,718%, from 11,000 to 1.3 million users in a single month.
Yet many telehealth services were overwhelmed by increasing patient demand and couldn’t respond to the volume of requests. People still struggled to access information and guidance when they needed it most.
Many patient services can’t be replaced by telehealth, such as childhood vaccines or cancer monitoring. Others which could be carried out virtually, such as monitoring blood pressure, were put on pause because CMS policies wouldn’t pay for home blood pressure monitors.
A survey from the Kaiser Family Foundation found that almost half of respondents said they or someone in their household had skipped or put off medical care due to COVID-19. Without regular in-person visits, a significant amount of medical care went undelivered, and 11% said that their conditions had worsened as a result.
Without reliable information, confusion reigns supreme
The “novel” nature of COVID-19 has left the general public confused and uncertain about what they can do, what they should do, and how to protect themselves and their loved ones, creating a space for dubious theories to circulate. Up to 30% of social media posts about the virus draw on unreliable sources, but patients aren’t always able to distinguish them, and now they can’t easily turn to their trusted physician for guidance.
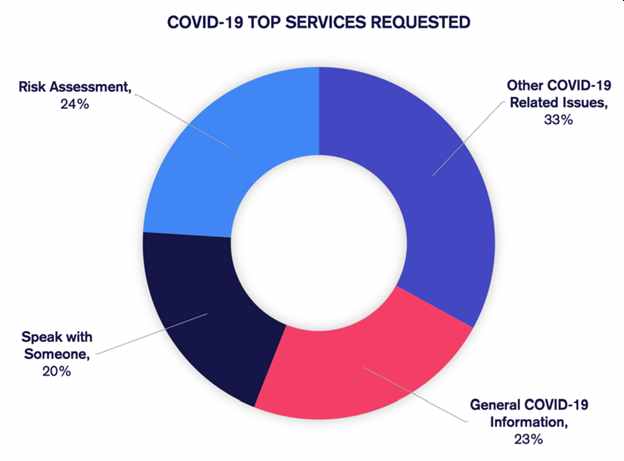
Hyro’s analysis of AI-patient conversations exposed an urgent need for trustworthy information. According to their findings:
● 23% of patients requested general information, often surrounding their medical provider’s COVID-19 readiness levels.
● Another 20% of patients requested to speak to someone.
● Within the category of “Other COVID-19 related issues”, 20% of patients asked about the number of cases, common symptoms, and safety concerns like whether it’s safe to go to work or not.
It’s worth pointing out that the information Hyro provides is easily extracted from certified resources and freely available information from the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and the healthcare organization’s own database.
COVID-19 tests head the list of patient concerns
Hyro’s data shows that testing is by far the biggest concern for patients. Some 56% of all “other COVID-19 related” interactions involved tests, and the phrases “tests, testing, and tested” topped the chart of the 10 most popular terms during patient conversations.

Although it’s understandable that Americans are concerned about coronavirus tests, it’s noteworthy that their questions are relatively simple – mainly about where to get a test and when, where, and how to receive results. So not only is there widespread demand for screening, there’s also a widespread lack of clarity about how to do so.
Healthcare messaging was lost in the chaos
13% of patient interactions with Hyro’s COVID-19 Virtual Assistants were concerned with hospital policy, urgent care policies, and rescheduling — topics that were difficult to address proactively by healthcare providers due to volatility surrounding the virus.
Common topics include confusion about hospital visitations and maternity-related questions. Expectant mothers don’t know how to prepare for their upcoming births, an uncertainty that has led to a rise in homebirth requests which could affect mother and baby safety.
Hospital administrators should take note of this, because delivering up-to-date information about policy will be key in convincing patients to feel safe returning to in-person care. Intermountain’s Cassia Regional Hospital Administrator Ben Smalley made the unsurprising observation that “The more we explain exactly what they should expect, the more comfortable [patients] are with the process.”
Frustrated patients could be the ones you didn’t expect
Demographic analysis of Hyro’s risk assessment tool, which triages patients’ symptoms, assesses their risk of infection, and provides immediate medical advice, reveals that most people using the tool are aged 30-50.
It’s unclear whether this means that this age group is more concerned than older people, or that older people are less inclined to find and use digital interfaces.
Either way, healthcare providers that may have targeted information primarily at the older age bracket should take note that middle-aged cohorts are at least equally worried, if not more so.
Keeping care providers in the conversation
The patient-healthcare provider relationship is a vital one, and when it’s disrupted, chaos ensues and medical care goes undelivered. Analysis of Hyro’s data reveals general frustration with lack of information and pressing desire for guidance, especially regarding testing. It’s crucial for healthcare providers to note the gaps in their service, places where messaging failed, and work to correct them before the widely predicted “second wave” arrives.
 April Klooster is a wellness coach on a mission to help individuals lead healthy and fulfilling lives by developing strength of spirit and body. Based in Red Bank, New Jersey, she works with clients from all over the globe. You can reach her on Twitter: https://twitter.com/AprilKlooster
April Klooster is a wellness coach on a mission to help individuals lead healthy and fulfilling lives by developing strength of spirit and body. Based in Red Bank, New Jersey, she works with clients from all over the globe. You can reach her on Twitter: https://twitter.com/AprilKlooster




